Pathogens and antimicrobial resistance amongst stroke patients in the intensive care unit: A five years review from Benin City, Nigeria
Accepted: 25 October 2021
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
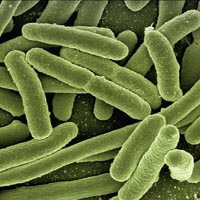
Severe stroke may necessitate intensive care unit admission, but there is a heightened risk of acquiring infection with use of ICU devices. Data regarding infection, pathogens and microbial resistance amongst stroke patients admitted into the ICU is scanty in Nigeria. This study aims to describe the infections, pathogens and antibiotics resistance pattern amongst stroke patients admitted into the ICU. It was a retrospective study. The ICU admission records of all stroke patients at the University of Benin Teaching Hospital from January 2014 to September 2019 were reviewed. The data obtained were the demographics, the types of stroke, results of microbiological studies on endotracheal aspirates, urine specimen, blood specimen, wound swab, vascular catheters, urinary catheters and the antibiogram pattern. One hundred and eight stroke patients were admitted into the ICU during the 5-year under review. The mean age was 61.8 with 51% being females and 52% having ischemic stroke. Seventy-five percent of the stroke patient had hospital acquired infection. Ventilator associated pneumonia accounted for 67.1% of infections, urinary tract infection was 22.8%, and blood stream infection 6.3% while 3.7% had infected decubitus ulcers. Microbial isolates were, Enterobacter sakazakii, accounting for 43.5%, Klebsiella pneumonia 13%, Escherichia coli 11.1%, and Proteus mirabilis 7.4% while 48% had Plasmodium falciparum infection. The micro-bacteria isolates were multi-antibiotics resistant, with the highest resistance for cotrimazole, cefuroxime and ceftazidime. The stroke patient in the ICU is susceptible to developing drug resistant hospital acquired infections, which could increase mortality. Ensuring minimal cases of ICU infection with continuous antimicrobial surveillance and robust antibiotics policy should be the goal.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/acbr.2021.162
https://doi.org/10.4081/acbr.2021.162



