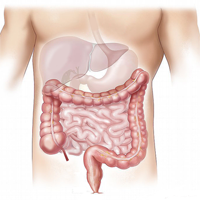
Metabolic changes in colorectal carcinomas are key factors for the early detection of neoplastic change
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 14 May 2021
Authors
Potential metabolic biomarkers have been developed by the use of modern analytical techniques and nanotechnology in metabolomics, providing insight into the pathophysiological basis and changes, tumorigenesis, and molecular mechanisms that underpin better therapeutic, monitoring, and prognostic evaluations of colon malignancies. This would allow early detection and characterization of malignant colon tumors and could reduce the risk of mortality and morbidity of colorectal carcinomas. Based on their association with certain metabolic pathways linked to malignancies, a number of tumor markers have been designed. Whereas some have been associated with only one cancer type, while others are associated with many different forms of cancer. No tumor marker has been found to have universal application as a metabolism-related marker; although some are circulating tumor markers found in blood, urine, stool, or other body fluids, others may be found in the specific tumors themselves. This paper addresses a number of associated metabolic changes linked to colorectal cancers and potential applications for disease condition diagnosis, monitoring, treatment, and prognosis.






