Morbidity patterns among medical admissions at Niger Delta University Teaching Hospital, Bayelsa State, Nigeria
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 29 April 2021
Authors
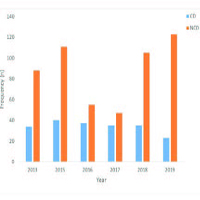
Hospital statistics on morbidity and mortality are essential in assessing disease burden, evaluation of health policies and health planning. The study aimed to determine the morbidity pattern and short-term outcome among medical admissions in the Niger Delta University Teaching Hospital (NDUTH), Bayelsa State, Nigeria. This retrospective 7-years disease audit was carried out in the medical wards of NDUTH, Bayelsa State, Nigeria. Information extracted included name and gender of patients, diagnoses and disease outcomes. One thousand, one hundred and twenty five (60.5%) females and seven hundred and thirty three (39.5%) males had complete records and were therefore used for the analysis. The mean age of the patients was 50.14±16.66 years with males being older (p<0.001). Non-Communicable Diseases (NCDs) accounted for a majority of cases (1270; 68.4%) while 588 (31.6%) were Communicable Diseases (CDs) NCDs were more prevalent among males and older individuals (p<0.03; p<0.001) and showed a rising trend over the years. CDs were however the leading cause of morbidities among females. The commonest diagnoses among males were retroviral disease, stroke, heart failure, pulmonary tuberculosis, diabetes and renal disease with women showing a similar trend except that heart failure replaced stroke as the second commonest morbidity while stroke came third, followed by diabetes, renal disease and hypertension. The all-cause mortality rates were 10.6% and 15.9% for females and males respectively. The major causes of mortality were infectious diseases and circulatory disorders for both genders. About 6.4% males and 3.8% females Left Against Medical Advice (LAMA). The pattern shows a rising prevalence of NCDs. Although CDs witnessed some decline, it however remained prevalent. The mortality rate was high while a good proportion LAMA. There is a need for strategic health programs to address this increasing tide of NCDs in our society, control CDs, and improve patient care while reducing mortality.






