Phototherapy services for newborns with jaundice: Availability and practices in Southeast Nigeria
Accepted: 24 November 2022
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
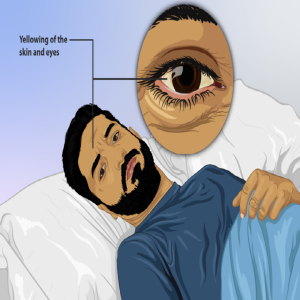
Severe neonatal hyperbilirubinemia remains a cause of neurologic damage in children in low-income countries. Phototherapy, which is the standard of care for neonatal hyperbilirubinemia is not only necessary but an essential neonatal service that should be readily available in all health facilities with maternal and newborn services. The study describes the availability and distribution of phototherapy service in secondary health facilities in Southeast Nigeria. This was a cross-sectional descriptive study carried out in four of the largest cities in Southeast Nigeria using purposive and convenient sampling methods. A questionnaire was administered and information regarding the availability of phototherapy machines, its use and availability of personnel was obtained. A total of 77 facilities were surveyed. Fifty-five (71.4%) of the studied facilities manage jaundice in their facility. Of these, 45/55 (81.8%) use phototherapy in the management of jaundice in newborns. The most used phototherapy is Light-Emitting Diode (LED) (42.2%). Others were fluorescent (26.6%), fabricated LED (11.1%) and fabricated fluorescent (20%). Routine serum bilirubin assay was done in 60 (77.9%) facilities even though majority was done in laboratories outside the facility. Non-invasive serum bilirubin monitoring was available in only two facilities. Only 21 (47.7%) had a servicing protocol for their phototherapy machines, and just 12 (27.7%) of these services were offered by a biomedical engineer. Phototherapy use in secondary health facilities is suboptimal. There is urgent need for states health authorities to collaborate with private health facilities especially those offering maternal and child services in provision of phototherapy machines and help in the training health workers for optimal management of neonatal hyperbilirubinemia.
Supporting Agencies
NoneHow to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/acbr.2022.240
https://doi.org/10.4081/acbr.2022.240



