Tuberculous parotitis in an immuno-competent adult: A rare clinical entity
Accepted: 22 December 2020
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
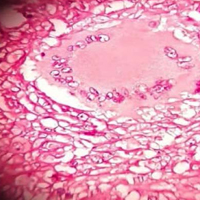
Majority of the cases of Tuberculosis (TB) occur in the pulmonary system, other extrapulmonary sites are rare, accounting for 15% of all TB cases. Among the extrapulmonary manifestations, TB parotitis is extremely rare, only few cases were reported in Africa despite the endemicity of the disease. We present a 23 years old man who developed a right infra-auricular swelling of three month duration, with no clinical or laboratory evidence of immunosuppression or TB in the lungs or other part of the body. High index of suspicion is required to diagnose this rare condition and the place of histological examination is imperative.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/pjm.2020.108
https://doi.org/10.4081/pjm.2020.108



